Electrical and Thermal Effects of Esophageal Temperature Probes on Radiofrequency Catheter Ablation of Atrial Fibrillation
Author Information: Juan J. Pérez, Andre D’Avila, Arash Aryana, and Enrique Berjano
Centro de Investigaci ́on e Innovaci ́on en Bioingenier ́ıa (Ci2B), Universitat Polit`ecnica de Val`encia, Valencia, Spain
Institutode Pesquisa em Arritmia Cardiaca, Hospital Cardiologico, Florianopolis, SC, Brazil
Regional Cardiology Associates and Dignity Health Heart and Vascular Institute, Sacramento, California, USA
Biomedical Synergy, Electronic Engineering Department, Universitat Polit`ecnica de Val`encia, Valencia, Spain
Publication Information
- Published in the Journal of Cardiovascular Electrophysiology, Volume 26, Issue 5
- May 2015
- Pages 558 – 584
- DOI: 10.1111/jce.12630
- Link: https://www.ncbi.nlm.nih.gov/pubmed/25648533
ABSTRACT:
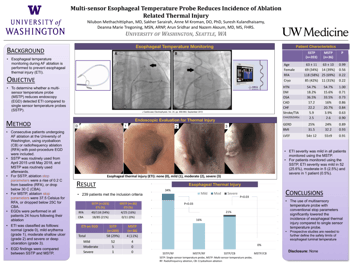
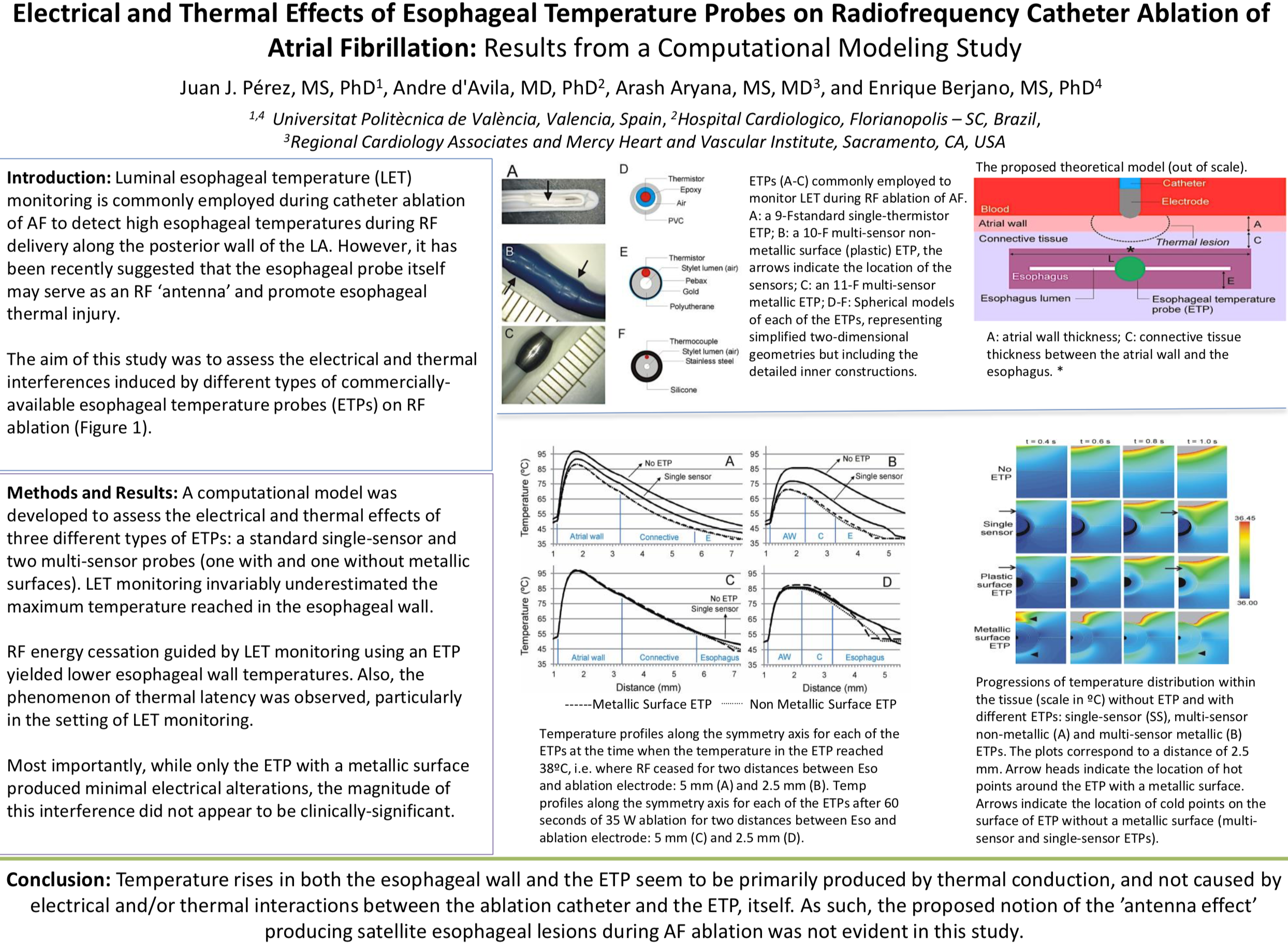
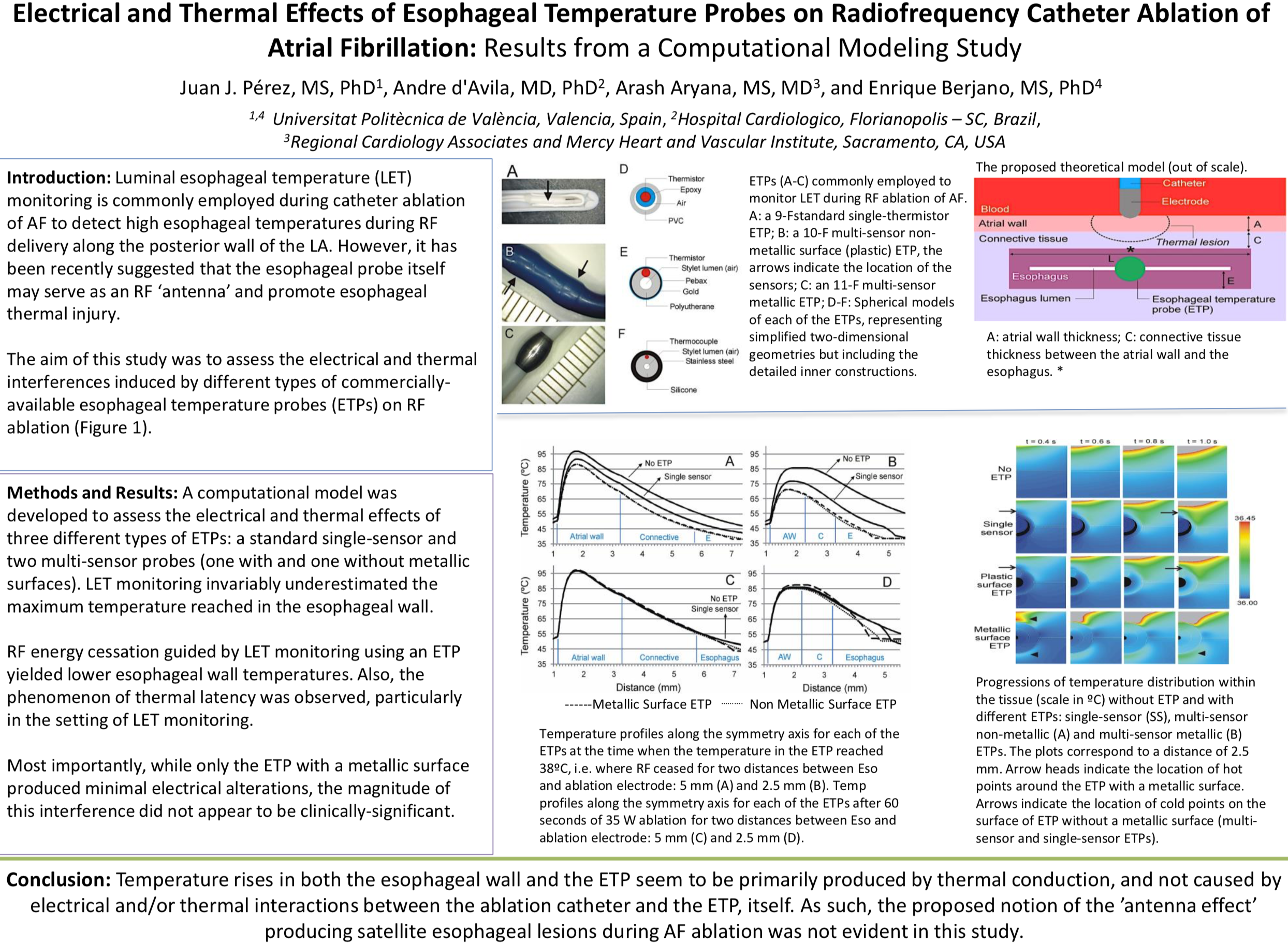
AIMS: Luminal esophageal temperature (LET) monitoring is commonly employed during catheter ablation of atrial fibrillation (AF) to detect high esophageal temperatures during radiofrequency (RF) delivery along the posterior wall of the left atrium. However, it has been recently suggested that in some cases the esophageal probe itself may serve as an RF “antenna” and promote esophageal thermal injury. The aim of this study was to assess the electrical and thermal interferences induced by different types of commercially available esophageal temperature probes (ETPs) on RF ablation.
METHODS AND RESULTS: In this study, we developed a computational model to assess the electrical and thermal effects of 3 different types of ETPs: a standard single-sensor and 2 multisensor probes (1 with and 1 without metallic surfaces). LET monitoring invariably underestimated the maximum temperature reached in the esophageal wall. RF energy cessation guided by LET monitoring using an
ETP yielded lower esophageal wall temperatures. Also, the phenomenon of thermal latency was observed, particularly in the setting of LET monitoring.Most importantly, while only the ETP with a metallic surface produced minimal electrical alterations, the magnitude of this interference did not appear to be clinically significant.
CONCLUSION: Temperature rises in both the esophageal wall and the ETP seem to be primarily produced by thermal conduction, and not caused by electrical and/or thermal interactions between the ablation catheter

.svg)
.svg)
.svg)